Ankle sprain

Ankle sprains are the most common form of trauma, with 2.2 million consultations per year in the United States alone (1). In France, ankle sprains are a frequent occurrence, with 6,000 cases per day (2). 70% of individuals may develop chronic instability over a short period after the initial injury. (1) This is why appropriate treatment is essential.
Although it is the most common form of trauma to this joint, the ankle can also be affected by fractures and inflammation. More rarely, osteoarthritis can occur.
The ankle
The ankle is a complex joint located between the leg and the foot. It is made up of a set of bones.
This includes the tibia, fibula and talus. The fibula is the smallest bone in the leg. The talus is the ankle bone. These bones are held together by several ligaments, which ensure the stability of the joint.
There are different types of ankle trauma. Traumatic injuries include sprains and fractures. These are injuries that affect the bones or ligaments..
On the other hand, we talk about musculotendinous pathologies when the lesions affect the tendons. These include tendinopathies.
Ankle sprains: a frequent trauma
Ankle sprains are caused by stretching or tearing of the ligaments in the joint. This mainly concerns the lateral ligaments, in 85% of cases (4,5). Ankle sprains can be classified as mild, with a stretched ligament, or severe, if the ligaments are ruptured and/or a fracture is added (5).
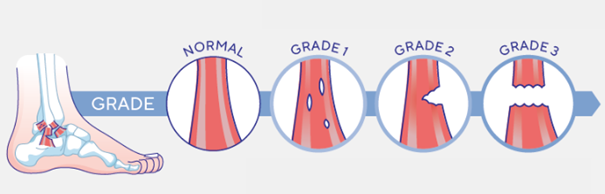
The different stages of severity of a sprain :
Mild sprain (stage I): The patient feels minimal pain (6), and there is discrete oedema (6). The patient also experienced minimal functional discomfort (6) and a proprioceptive deficit. You can use the Thuasne MalleoAction splint to immobilise a sprain at this stage.
Moderate sprain (stage II): The patient feels more intense pain (6), and there is visible swelling and bruising (7). There is definite functional discomfort (7) and slight instability (7). For immobilisation of a sprain at this stage, you can use the MalleoDynastab BOA splint from Thuasne.
Severe sprain (stage III): Persistent pain (6), significant swelling and extensive bruising (6). Significant functional discomfort (6). For immobilisation of a sprain at this stage, you can use the Thuasne XLR8 walking boot.
Certain factors are more likely to lead to an ankle sprain:
Playing sports: contact sports (football, etc.) and pivot sports, in which changes of direction are abrupt (tennis, basketball, etc.) (8) 50% of ankle sprains occur during sports activities. (19) Walking on uneven ground (risk of slipping) or on uneven surfaces (9) Wearing unstable shoes (high heels), ill-adapted to the activity, or worn-out shoes (10,11) Structural abnormalities, such as flat feet or legs of unequal length. (8)
Sprained ankle: what to do and how to treat it?
Relieving an ankle sprain involves resting with the affected limb elevated, applying ice to relieve pain, applying a compression bandage (12), which is what is known as the RICE protocol, taking painkillers (13) and using walking sticks to get around. The ankle must be immobilised with splints or walking boots for 3 to 6 weeks (14). For rehabilitation and resumption of activity, physiotherapy and wearing an ankle brace are recommended (6). In the case of a fracture, surgery, walking boots or a plaster cast may be necessary. If you think you have sprained your ankle, do not hesitate to consult a doctor for a clinical examination.
What is the role of the physiotherapist in ankle sprains?
The physiotherapist plays a key role in the rehabilitation and recovery from an ankle sprain. Their intervention aims to reduce pain, restore mobility and prevent recurrence through a progressive and personalised approach.
1. Reduction of pain and swelling
In the initial phase, the physiotherapist may recommend drainage techniques, cryotherapy and gentle exercises to limit inflammation and improve the patient's comfort. (15)
2. Restoration of mobility and muscle strengthening
Once the pain has stabilised, mobility and progressive strengthening exercises are introduced to restore joint range of motion and improve ankle stability. Adapted balance exercise programmes have been shown to be effective in reducing the risk of recurrence. (15)
3. Improving balance and proprioception
Sprains can alter proprioception (perception of the position of the ankle in space), thus increasing the risk of further injury. The physiotherapist will set up specific exercises to strengthen neuromuscular control and avoid chronic instability. (15)
4. Prevention of recurrence
Appropriate care significantly reduces the risk of further sprains. Post-sprain rehabilitation exercises halve the recurrence rate after 12 months. (16)
FAQ :
Why wear a brace when you feel pain in your ankle?
Wearing a brace when you feel pain in your ankle, due to a sprain for example, allows you to immobilise the ankle in order to limit movement and provides stability to the joint. This is part of the RICE ‘protocol’ (Rest, Ice, Compression, Elevation) (see our dedicated article)
Why do I always have a sore ankle?
If you feel pain that suggests a sprain, fracture, tendonitis or any other condition listed in this article, consult a healthcare professional for a diagnosis and optimal treatment. A sprain that is not properly treated can lead to fragility in the future.
Sprained ankle: How long before I can return to sport?
Returning to sport after a sprained ankle depends on the severity of the sprain (17): For a mild sprain, it will take 1 to 3 weeks. For a moderate sprain, it will take 4 to 6 weeks. In the case of a serious sprain, it takes between 6 weeks and 3 months.
In cases of mild to moderate sprains (grade I or II sprains), walking can be considered, but with precautions. One study showed that persistent pain when walking after a sprain was an indicator of poor long-term recovery. (18)
In these cases, the use of crutches or a stabilising splint is recommended to avoid putting strain on the injured ankle. (6)
In the case of a serious sprain (grade III), walking immediately after the injury can aggravate the injury and slow down recovery. One study has shown that the absence of adequate stabilisation after a severe sprain can increase the risk of recurrence and chronic pain. (18)
When should you start walking again after a sprain?
In the first few days, avoid excessive weight-bearing and prioritise rest with a compression bandage. Walking can be resumed gradually when the pain subsides and the foot is stable enough. Exercise rehabilitation is essential to prevent recurrence and strengthen the injured ligaments. (15)
Sources :
1. Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA. Epidemiology of Ankle Sprains and Chronic Ankle Instability. J Athl Train. 2019 Jun;54(6):603-610. doi:10.4085/1062-6050-447-17. Epub 2019 May 28. PMID: 31135209; PMCID: PMC6602402
2. POIRI, A., CHALOPIN, A., DECANTE, C., MAYRARGUE, E., HAMEL, A., RENNES UNIVERSITY HOSPITAL, DEPARTMENT OF PEDIATRIC SURGERY, F-35033 RENNES, FRANCE, Pediatric surgery department, Brest University Hospital, & Pediatric surgery department, Nantes University Hospital. (n.d.). Are ankle sprains always benign? https://sofop.org/medias/files/textes_scientifiques/monographies/2022/EN/02.pdf COMMISSION NATIONALE D’EVALUATION DES DISPOSITIFS MEDICAUX ET DES TECHNOLOGIES DE SANTE. (n.d.). Avis de la CNEDiMTS - A2T, orthèse stabilisatrice de cheville. https://www.has-sante.fr/upload/docs/evamed/CEPP-5487_A2T_15_mai_2018_(5487)_avis.pdf
3. COMMISSION NATIONALE D’EVALUATION DES DISPOSITIFS MEDICAUX ET DES TECHNOLOGIES DE SANTE. (n.d.). Avis de la CNEDiMTS - A2T, orthèse stabilisatrice de cheville. https://www.has-sante.fr/upload/docs/evamed/CEPP-5487_A2T_15_mai_2018_(5487)_avis.pdf
4. Cerezal, A., Ocampo, R., Llopis, E., & Cerezal, L. (2023). Ankle Instability Update. Seminars in Musculoskeletal Radiology, 27, 231 - 244. https://doi.org/10.1055/s-0043-1767767
5. Melanson SW, Shuman VL. Acute Ankle Sprain. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459212/
6. Haute Autorité Santé ,” DISPOSITIFS de COMPRESSION/CONTENTION médicale à usage individuel Utilisation en ORTHOPÉDIE/ RHUMATOLOGIE/ TRAUMATOLOGIE”; Octobre 2012 (consulté le 07/10/2024). HAS : https://www.has-sante.fr/jcms/c_1318289/fr/dispositifs-de-compression/contention-medicale-a-usage-individuel-utilisation-en-orthopedie/rhumatologie/traumatologie
7. Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician. 2001 Jan 1;63(1):93-104. Erratum in: Am Fam Physician 2001 Aug 1;64(3):386. PMID: 11195774.
8. Raj MA, Tafti D, Kiel J. Pes Planus. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430802/
9. B. J. McCriskin, K. L. Cameron, J. D. Orr, and B. R. Waterman, “Management and prevention of acute and chronic lateral ankle instability in athletic patient populations,” World J. Orthop., vol. 6, no. 2, pp. 161–171, 2015, doi: 10.5312/wjo.v6.i2.161
10. Beynnon BD, Murphy DF, Alosa DM. Predictive Factors for Lateral Ankle Sprains: A Literature Review. J Athl Train. 2002 Dec;37(4):376-380. PMID: 12937558; PMCID: PMC164368.
11. Jessica A. Dobson, Diane L. Riddiford-Harland, Alison F. Bell, Julie R. Steele, Work boot design affects the way workers walk: A systematic review of the literature, Applied Ergonomics, Volume 61, 2017, Pages 53-68, ISSN 0003-6870, https://doi.org/10.1016/j.apergo.2017.01.003.
12. Van den Bekerom MP, Struijs PA, Blankevoort L, Welling L, van Dijk CN, Kerkhoffs GM. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults? J Athl Train. 2012 Jul-Aug;47(4):435-43. doi: 10.4085/1062-6050-47.4.14. PMID: 22889660; PMCID: PMC3396304.
13. Vuurberg G, Hoorntje A, Wink LM, et alDiagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guidelineBritish Journal of Sports Medicine 2018;52:956. https://doi.org/10.1136/bjsports-2017-098106
14. Prado, M., Mendes, A., Amodio, D., Camanho, G., Smyth, N., & Fernandes, T. (2014). A Comparative, Prospective, and Randomized Study of Two Conservative Treatment Protocols for First-episode Lateral Ankle Ligament Injuries. Foot & Ankle International, 35, 201 - 206. https://doi.org/10.1177/1071100713519776.
15. Ruiz-Sánchez FJ, Ruiz-Muñoz M, Martín-Martín J, Coheña-Jimenez M, Perez-Belloso AJ, Pilar Romero-Galisteo R, Gónzalez-Sánchez M. Management and treatment of ankle sprain according to clinical practice guidelines: A PRISMA systematic review. Medicine (Baltimore). 2022 Oct 21;101(42):e31087. doi: 10.1097/MD.0000000000031087. PMID: 36281183; PMCID: PMC9592509.
16. Bleakley, C., Dischiavi, S., Taylor, J., Doherty, C., & Delahunt, E. (2017). O30 Rehabilitation reduces re-injury risk post ankle sprain, but there is no consensus on optimal exercise dose or content: a systematic review and meta-analysis. British Journal of Sports Medicine, 51, A12 - A12. https://doi.org/10.1136/bjsports-2017-anklesymp.30.
17. https://www.ameli.fr/assure/sante/themes/entorse-cheville/reprise-activites-evolution. (Consulté le 25/02/2025)
18. Terrier, P., Piotton, S., Punt, I., Ziltener, J., & Allet, L. (2021). Facteurs prédictifs de récupération après une entorse latérale aiguë de la cheville : une étude longitudinale. Sports , 9. https://doi.org/10.3390/sports9030041
19. Waterman, Brian R. MD1; Owens, Brett D. MD2; Davey, Shaunette DO1; Zacchilli, Michael A. MD1; Belmont, Philip J. Jr. MD1. The Epidemiology of Ankle Sprains in the United States. The Journal of Bone & Joint Surgery 92(13):p 2279-2284, October 6, 2010. | DOI: 10.2106/JBJS.I.01537
Crédit photo : Mladen Mitrinovic / Shutterstock