Osteoarthritis of the knee: the physiotherapist’s role
The effective treatment of osteoarthritis of the knee (or gonarthrosis) requires multidisciplinary management. Among the various healthcare professionals involved, the physiotherapist may play a particularly important role. But when is their input required? And what is there exact role?
Over the years, physiotherapy has come to play a crucial part in the management of osteoarthritis of the knee, whatever its stage. In young people, it can help improve detection of the condition. At more advanced stages, it can also limit, delay or prepare for surgery(1).
“Passive” mobilisation of the knee (when only the practitioner is active, with the patient just letting it happen) in flexion and extension positions helps maintain good joint health(1). In concrete terms, the therapist manipulates the patient's leg, bending and stretching it in turn. This also relieves strain on the joint and may even improve cartilage nutrition(2)!
The physiotherapist can also help with “active” postures (here the patient generates the movement) in extension or flexion positions. These help combat the loss of mobility associated with the condition, and improve the joint’s range of motion(1).
Stretching certain muscle groups (such as the hamstrings or quadriceps) can improve the range of motion of the knee if extension or flexion are limited(1). Like postures, these stretching exercises can be done passively with the help of the physiotherapist, or the patient can do them alone at home as part of a self-education programme. Using a diversity of different positions can increase the benefits.

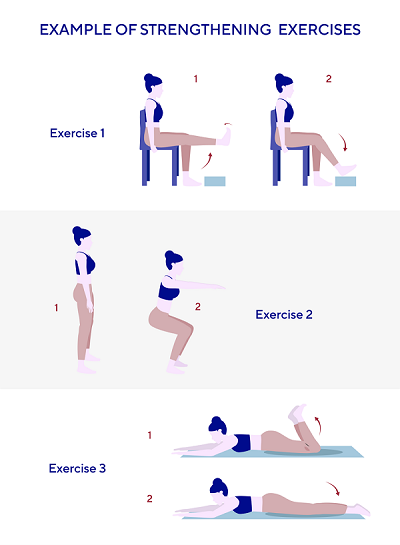
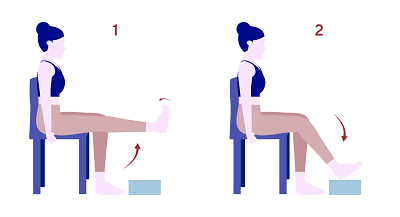
Osteoarthritis of the knee can contribute to weakness in the muscles that stabilise the knee (quadriceps, hamstrings). That is why muscle strengthening exercises are necessary. When it comes to types of strengthening exercises, there are two, contrasting main trends(1):
• In English-speaking countries, dynamic (moving) strengthening exercises are used against little or no resistance, sometimes combined with endurance work;
• In France, isometric strengthening exercises (with no movement during the contraction) against resistance is preferred.
Despite their differences, these two trends agree on the importance of progressive stepping up of the work required, in order to avoid painful phenomena(1).
A cycle ergometer (exercise bike) is also recommended for maintaining good knee health(1). In addition, different areas of the body (ankle, knee or hip) can be mobilised by lowering or raising the saddle.
Massages by physiotherapists play an important role in the treatment of OA of the knee. These massages meet several objectives(1):
• They help stretch the muscles (deep kneading techniques)
• They promote venous and lymphatic return (gentle and surface massage movements)
• They alleviate pain in the knee (pain-relieving)
“Physical agents” (noise, vibrations, electricity, rays, pressure, etc.) can also be used by physiotherapists to treat osteoarthritis of the knee. Among these, only TENS (transcutaneous electrical nerve stimulation) and balneotherapy appear to have pain-relieving effects(1).
The use of cold may improve joint range of motion and reduce pain during inflammatory flare-ups(1). While heat helps loosen and relax muscles outside inflammatory flare-ups(1).
Patient education is an educational approach that aims to make patients active and autonomous players in the care of their condition. Patients work together with their physiotherapist to develop an appropriate and acceptable treatment programme. In a condition like osteoarthritis of the knee, patient education relating to lifestyle and diet is crucially important(1).
If you have any questions, ask your doctor for advice.
1. Estrade J-L. Kinésithérapie de la gonarthrose fémorotibiale non opérée. EMC - Kinésithérapie – Médecine physique – Réadaptation. 2008;4(3):1-32.
2. Sharma G and al, Differential effects of cyclic and static pressure on biochemical and morphological properties of chondrocytes from articular cartilage, clin biomech, 2007, p 248-255.