Osteoarthritis of the knee: symptoms and treatments of gonarthrosis
Our knees play an essential role when it comes to supporting our bodies and keeping us mobile. These joints support our weight and movements in all our routine activities. Hence a degenerative cartilage disease like osteoarthritis of the knee (also known as OA or gonarthrosis) can quickly become incapacitating in our everyday lives.
The anatomy of the knee
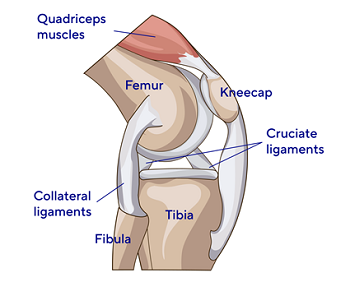
The extremities of the bones in the knee joint - the femur, tibia and kneecap (also called the patella) - are covered by cartilage. This cartilage enables good joint mobility. Without it, bones would come into contact with one another. The cartilages of the knee joint also include meniscus, a kind of small cushion improving the contact between the cartilages of the femur and the tibia and contributing to the joint’s stability. The joint is also surrounded by an envelope that helps lubricate and nourish the cartilage: the synovial capsule.
What is osteoarthritis of the knee (gonarthrosis)?

Osteoarthritis of the knee indicates degeneration of the cartilage in the knee joint. The condition primarily develops with age and progresses via episodic flare-ups.
Excessive pressure on the cartilage damages it: it begins to wear and is then gradually destroyed until there is none left. Osteoarthritis can also be accompanied by the formation of bony outgrowths on the edges of the joint, called “osteophytes”.
At the same time, the synovial capsule starts to become inflamed. This can cause fluid to leak out, causing what is known as “synovial effusion”.
The different types of osteoarthritis of the knee
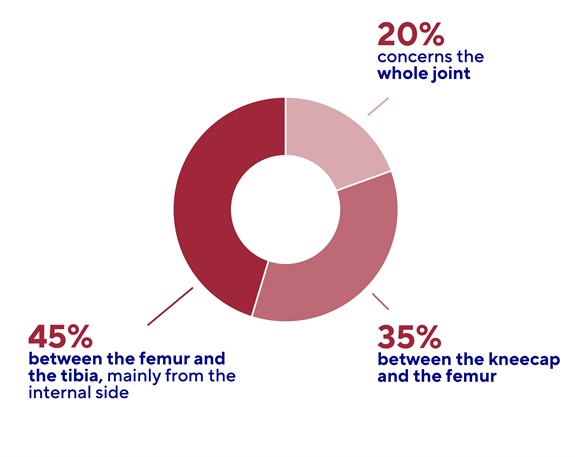
There are three types of osteoarthritis of the knee, depending on where the damaged cartilage is located(1):
• Femorotibial osteoarthritis : The most common type (45 to 50% of cases) is arthritis between the femur and the tibia. This is mainly internal (or medial), meaning that it affects the inside of the knee, but it can also be external (or lateral), affecting the outside of the knee.
• Patellofemoral osteoarthritis : It is located between the kneecap and the femur (35% of cases).
• Tricompartmental osteoarthritis : It occurs when the whole joint is affected (15 to 20% of cases). This is known as of the knee.
Some data concerning osteoarthritis of the knee
• The gonarthrosis affects 22.9% of people over the age of 40.
• Every year, 86 million people develop osteoarthritis of the knee.
• It affects more women than men.
Symptoms of osteoarthritis of the knee : pain...
Osteoarthritis of the knee may be asymptomatic at the start: it is discovered following an X-ray but does not cause any pain. As it progresses or worsens, pain may occur during routine activities. The pain is described as “mechanical”, meaning that it increases when the joint is used (walking, heavy lifting, going up or down stairs, etc.) and is alleviated by rest. It is absent at night, except when changing position in bed. In the morning, the knee may seem stiff after first getting out of bed and take a little time to “loosen up”.
A painful flare-up generally occurs when a fragment of cartilage becomes detached. This triggers synovial effusion. As a result, the knee begins to swell, causing pain and impeding mobility.
The pain varies depending on the type of osteoarthritis of the knee: diffuse in the event of femorotibial OA and predominantly at the front of the knee in the event of patellofemoral OA. Furthermore, the condition is often bilateral and symmetrical: both knees are affected in the same way(1).
What are the causes of osteoarthritis of the knee?
Osteoarthritis of the knee is a primarily age-related degenerative condition. Its prevalence in the under 40s is less than 10%, whereas it affects 30% of the over 60s and half of all people over the age of 80!(2)
There are more specific risk factors for OA of the knee, such as:
• Being overweight or obese, since this increases strain on the knee joints.
• A lack of physical exercise, which weakens the joints.
• Old joint injuries (dislocation, serious sprain, ligament rupture), sometimes related to work activities (heavy lifting, working on knees) or sports (repeated sudden movements), which weaken the joint(3)
There are also genetic predispositions to certain types of osteoarthritis. Metabolic diseases, such as gout, or inflammatory conditions like rheumatoid arthritis can also promote its development.
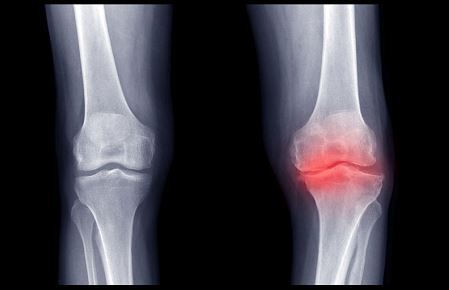
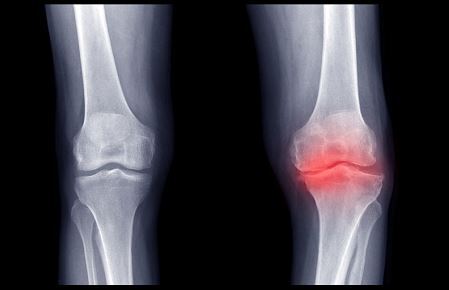
Diagnosis of gonarthrosis
Diagnosis of osteoarthritis of the knee is initially based on physical examination: the doctor looks for the presence of effusion in the joint and a limited range of motion in the knee’s movements. The doctor will also seek to assess the patient’s level of day-to-day pain and disability.
Knee X-rays are systematically performed to identify any elements suggestive of osteoarthritis, such as osteophytes or the joint space width (space between the femur and the tibia).
Treatments for osteoarthritis of the knee
Knee osteoarthritis is a chronic condition: there is no cure. Therefore its treatment is symptomatic. The aim is to relieve pain, restore joint mobility and avoid isolation and withdrawal.
The treatment of osteoarthritis of the knee involves several components. First-line treatment consists of non-medicinal management, such as lifestyle and dietary measures (including weight loss), the use of braces or walking sticks, thermal spa therapy, etc.
Medication is used as second-line treatment. Depending on the stage of the disease, this may be accompanied by infiltrations and tidal lavages (washing out the knee joint). As a last resort, surgical knee joint replacement may be considered.
Treatment by physiotherapy and regular physical activity

Regular physical activity and physiotherapy exercises offer numerous benefits, such as better weight control, strengthening of the muscles and loosening of tendons in the knee joint. The aim is to maintain maximum mobility. Physical activity should be combined with a balanced diet and follow the 3R rule: Rational, Regular and Reasonable.
Relieving osteoarthritis of the knee with medication
Analgesics and anti-inflammatories may be prescribed to relieve pain and limit loss of mobility in the event of flare-ups. Injections may also be administered into the joints. Slow-acting anti-arthritic drugs are available for long-term, disease-modifying therapy. But their efficacy is debated and the funding of these drugs is being called into question in several countries.
The management of osteoarthritis of the knee requires a multidisciplinary medical team: general practitioner, rheumatology specialist, physiotherapist and, when surgery is required, orthopaedic surgeon.
If you have any questions, ask your doctor for advice.
1. Collège français des enseignants en rhumatologie. Arthrose. Website: Cofer. Paris; 2017
2. Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. Published 2020 Nov 26. doi:10.1016/j.eclinm.2020.100587
3. Literature Review of Risk Factors, Evaluation Instruments, and Care and Service Interventions for Knee Osteoarthritis